Knee Physical Therapy – Expert Care for Optimal Joint Health
The knee is the largest joint in the human body and one of the most commonly injured structures. Positioned between two long bones – the femur and the tibia – the knee relies primarily on ligaments, tendons, and surrounding muscles to maintain stability. Unlike ball-and-socket joints, the knee’s bony anatomy offers limited inherent stability, making it susceptible to acute injuries, age-related wear, and degenerative changes. Without proper care, knee pain can range from mild discomfort to severe disability that affects daily activities and athletic performance.
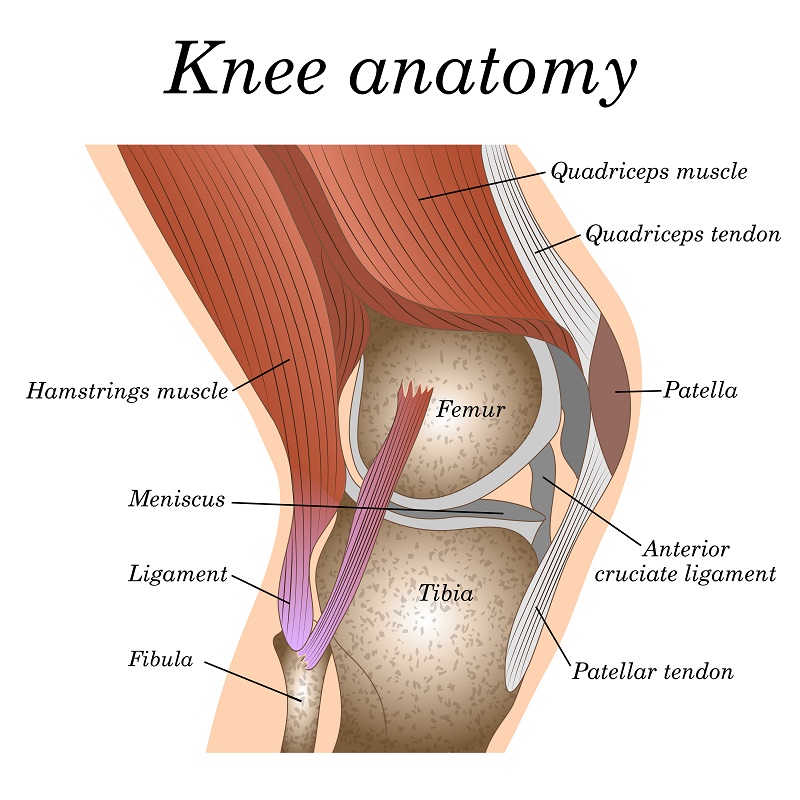
Knee Anatomy & Common Injury Mechanisms
The knee joint comprises the femur (thigh bone), tibia (shin bone), and patella (kneecap). Four primary ligaments – the anterior cruciate ligament (ACL), posterior cruciate ligament (PCL), medial collateral ligament (MCL), and lateral collateral ligament (LCL) – provide major stabilization. The menisci, two C-shaped cartilage structures, act as shock absorbers between the femur and tibia. Surrounding muscles, including the quadriceps, hamstrings, and calf muscles, further support the joint through dynamic stabilization.
Because the knee bears significant load during activities like walking, running, jumping, and squatting, it is prone to injury. Examples include:
- Traumatic Injuries: Sudden impact or twisting motions can cause ligament tears, meniscal tears, or fractures.
- Overuse Injuries: Repetitive stress from running or jumping can lead to tendonitis, bursitis, or patellofemoral pain syndrome.
- Degenerative Changes: Age-related wear of cartilage can result in osteoarthritis, causing pain, stiffness, and reduced range of motion.
- Biomechanical Faults: Muscle imbalances, poor alignment, or improper training techniques can contribute to conditions such as ITB syndrome or patellar instability.
Why Choose OrthoRehab Specialists for Knee Therapy?
OrthoRehab Specialists is a therapist-owned and operated practice serving the Twin Cities area for over 25 years. Our physical therapists specialize in evidence-based knee rehabilitation, drawing from advanced training and ongoing continuing education. Key differentiators include:
- Hands-On, One-on-One Care: You work directly with the same licensed physical therapist at every visit for consistent feedback and progress tracking.
- Therapist Expertise: Our clinicians hold advanced certifications in orthopedic manual therapy, sports rehabilitation, and functional movement assessment.
- Comprehensive Evaluation: We perform thorough assessments – ranging from joint mobility and strength testing to gait analysis and dynamic movement screens – to identify underlying dysfunctions.
- Customized Treatment Plans: Each program is tailored to your specific condition, goals, and activity demands, whether you are recovering from ACL surgery or aiming to return to high-level sports.
- State-of-the-Art Facilities: Our clinics feature modern equipment for functional training, balance drills, and advanced therapeutic modalities such as dry needling and blood flow restriction training.
- Collaborative Approach: We communicate regularly with referring physicians, surgeons, and athletic trainers to ensure coordinated care and optimal outcomes.
Comprehensive Knee Evaluation Process
Before designing a treatment plan, our therapists conduct a detailed evaluation that includes:
- Patient Interview: We discuss your history, symptom patterns, activity level, and functional goals – whether you want to walk without pain, return to sports, or delay a recommended knee replacement.
- Postural & Alignment Assessment: We analyze static and dynamic alignment of the pelvis, hip, and lower extremity to identify biomechanical issues contributing to knee dysfunction.
- Joint Mobility Testing: We measure joint range of motion in flexion, extension, and rotation, noting any restrictions or hypermobility that may affect knee mechanics.
- Ligament & Meniscus Screening: Orthopedic special tests such as Lachman’s test, McMurray’s test, and varus/valgus stress tests identify ligamentous integrity and meniscal injury.
- Muscle Strength & Flexibility: We assess quadriceps, hamstrings, calf, and hip muscle strength, as well as flexibility of the iliotibial band, hamstrings, and calf complex to detect imbalances.
- Functional Movement & Gait Analysis: Video and observational analyses of squatting, lunging, walking, and single-leg stance reveal compensations and movement faults that can exacerbate knee pain.
- Balance & Proprioception Screening: Tests such as single-leg balance and dynamic stability tasks evaluate neuromuscular control vital for knee stability.
Personalized Treatment Interventions
Following the evaluation, our clinicians develop a customized plan that may include:
- Manual Therapy: Techniques such as soft tissue mobilization, joint mobilizations, and connective tissue manipulation reduce pain, improve joint glide, and enhance circulation.
- Therapeutic Exercises: Progressive strengthening of the quadriceps, hamstrings, gluteal complex, and calf muscles restores stability and improves functional movement patterns.
- Neuromuscular Re-education: Balance drills, proprioceptive training, and dynamic stability exercises help retrain the neuromuscular system for improved joint control.
- Gait Retraining: We analyze and correct walking and running mechanics to reduce abnormal loading on the knee, preventing future injuries.
- Biomechanical Corrections: Custom foot orthotics, taping techniques, or bracing may be used to correct alignment issues and offload stress from injured knee structures.
- Modalities: When indicated, we utilize cold laser therapy, ultrasound, electrical stimulation, and kinesio taping to reduce inflammation and facilitate tissue healing.
- Functional Training: For athletes, we integrate sport-specific drills, plyometrics, and agility training to safely progress you back into competition.
- Patient Education: We provide guidance on activity modification, proper warm-up and cool-down routines, and home exercises to empower you in your recovery.
Knee Conditions We Treat
Our specialists treat a wide spectrum of knee pathologies, including but not limited to:
- ACL Injuries: Ruptures or sprains of the anterior cruciate ligament, often requiring pre- and post-operative rehabilitation to restore stability and strength.
- MCL Injuries: Medial collateral ligament sprains or tears caused by valgus stress. Treatment includes bracing, targeted strengthening, and neuromuscular training.
- LCL Injuries: Lateral collateral ligament damage due to varus stress. We focus on stability through hip and thigh strengthening and controlled loading protocols.
- PCL Injuries: Posterior cruciate ligament dysfunction affecting knee kinematics. Rehabilitation includes proprioceptive drills and quadriceps strengthening to compensate for ligament insufficiency.
- Meniscus Injuries: Tears in the medial or lateral meniscus that cause joint locking, clicking, and pain. Our protocols range from conservative management to post-surgical rehab to restore range of motion and function.
- Patellofemoral Syndrome: Pain arising from maltracking of the kneecap, often linked to quadriceps imbalance or hip weakness. Treatment emphasizes VMO activation, hip abductor strengthening, and gait retraining.
- Patellar Tendinitis: Overuse condition of the patellar tendon causing anterior knee pain. We implement eccentric loading exercises, soft tissue techniques, and gradual return-to-sport planning.
- Chondromalacia: Softening or degeneration of the articular cartilage under the patella. Our interventions include manual therapy, quadriceps strengthening, and activity modification to reduce compressive forces.
- Osteoarthritis: Degenerative joint disease leading to cartilage breakdown, stiffness, and pain. We use joint mobilizations, low-impact strengthening, and functional adaptability training to maintain mobility and delay progression.
- Knee Instability: Feeling of giving way due to ligamentous laxity or neuromuscular deficits. We emphasize closed-chain strengthening, balance training, and bracing when necessary to restore confidence in movement.
- Articular Cartilage Defects: Focal defects in cartilage requiring specialized loading and unloading strategies to facilitate tissue healing and prevent further degeneration.
- Knee Replacement Rehabilitation: Pre-operative conditioning and post-operative protocols to achieve optimal range of motion, strength, and functional independence after total or partial knee arthroplasty.
- Baker’s Cyst: Fluid-filled swelling behind the knee often associated with meniscal tears or arthritis. We address underlying pathology, perform manual drainage, and work on joint mobility to reduce cyst recurrence.
- Bursitis: Inflammation of bursae around the knee resulting from repetitive stress or direct trauma. Treatment includes soft tissue mobilization, anti-inflammatory modalities, and activity modifications.
- Hoffa’s Fat Pad Syndrome: Irritation of the infrapatellar fat pad causing anterior knee pain. We use manual therapy techniques, hip and core strengthening, and gradual loading to alleviate symptoms.
- IT Band Syndrome: Tightness and friction of the iliotibial band over the lateral femoral epicondyle. Our approach includes foam rolling, hip abductor strengthening, and gait analysis to correct biomechanical faults.
- Peripheral Nerve Entrapment: Compression of nerves like the saphenous nerve causing radiating knee pain. Interventions include neural mobilization, manual therapy, and ergonomic adjustments.
- Plica Syndrome: Irritation of the synovial plica in the knee joint causing clicking and discomfort. We address inflammation, perform manual mobilizations, and prescribe hip and quadriceps strengthening.
- Tendon Ruptures: Complete tears of the quadriceps or patellar tendon requiring surgical repair and specialized post-operative rehabilitation to restore function and strength.
- Fractures: Tibial plateau or patellar fractures treated with immobilization or surgery. Our protocols focus on edema control, range of motion restoration, and progressive strengthening as healing permits.
Knee Physical Therapy Locations
Our downtown clinic and suburban clinic both offer specialized knee care. Each facility features private treatment rooms, dedicated rehabilitation equipment, and therapeutic exercise areas designed to meet the needs of knee injury patients. Whether you require post-operative rehabilitation, non-operative conservative care, or advanced performance training, our teams are equipped to support you.
Getting Started: Your First Knee Therapy Visit
Prior to your appointment, please prepare the following:
- Insurance Card & Photo ID: We will verify your benefits and confirm coverage. If self-paying, we offer transparent cash rates and flexible payment plans.
- Comfortable Athletic Attire: Wear shorts or athletic pants and a fitted top to allow full range-of-motion assessment. Athletic shoes with support are recommended, especially for gait evaluation.
- Relevant Medical Records: Bring any recent imaging reports (X-ray, MRI, CT) or surgical notes. If unavailable, we can request records electronically from your provider with your consent.
- List of Medications & Medical History: Include all prescription and over-the-counter medications, allergies, and chronic conditions to ensure safe and coordinated care.
- Assistive Devices & Braces: If you currently use a knee brace, crutches, cane, or other devices, bring them to your appointment. We will assess their impact on your mobility and recommend any necessary adjustments.
- Questions & Goals: Write down specific concerns, questions, or functional goals such as returning to running, resuming work duties, or achieving pain-free walking.
What to Expect During Your Evaluation
Your first session will last approximately 60 minutes and include the following steps:
- Patient Interview: We discuss the history of your knee condition, including onset, duration, and any prior treatments. We also explore how your symptoms affect work, sports, and daily activities.
- Physical Assessment: The therapist measures joint range of motion in flexion, extension, and rotation. We assess muscle strength (quadriceps, hamstrings, hip abductors), flexibility (hamstrings, calf muscles, iliotibial band), and joint stability through manual ligament tests.
- Functional Movement Screening: We analyze your squatting, lunging, stepping, and walking patterns to identify movement faults and compensations. Video analysis may be used to capture gait biomechanics in real time.
- Balance & Proprioception Tests: Single-leg stance, star excursion balance test, and dynamic stability drills help identify neuromuscular control deficits critical for knee stability.
- Objective Measurements: When indicated, we measure limb circumference, girth, or limb length differences. Functional tests – such as the single-leg hop test or timed stair climb – provide baseline data for tracking progress.
- Collaborative Goal Setting: After reviewing assessment findings, we establish realistic short-term and long-term goals tailored to your lifestyle and functional demands. Goals may include walking without pain, returning to sports, or avoiding knee replacement surgery.
- Treatment Planning: Based on your evaluation, the therapist outlines a customized plan that may include manual therapy, therapeutic exercises, functional training, patient education, and a home exercise program. We discuss expected timelines, session frequency, and measurable milestones to monitor progress.
Follow-Up Visits & Progress Monitoring
During subsequent visits, your therapist focuses on implementing and progressing your treatment plan. We track improvements in range of motion, muscle strength, balance, and functional performance. Objective measures – such as goniometer readings, isometric strength tests, and functional movement screens – guide our decisions. As you achieve each milestone, we refine exercises, advance manual techniques, and incorporate higher-level functional drills to ensure continued progress and prevent setbacks.
Cancellation & Rescheduling Policy
We understand that schedules can change. If you need to cancel or reschedule your appointment, please provide at least 24 hours’ notice. Late cancellations – less than 24 hours’ notice – and no-shows may incur a fee. If you have an emergency, contact us as soon as possible so we can accommodate you without penalty.
Frequently Asked Questions (FAQ)
Do I need a doctor’s referral to start knee therapy?
No. Minnesota’s direct access law allows you to schedule an evaluation without a referral. If your insurance plan requires a prescription or pre-authorization, we will inform you and assist with any necessary paperwork.
How long is the initial evaluation?
Your first session usually lasts about 60 minutes. This includes intake forms, a comprehensive interview, physical assessments, goal setting, and development of an individualized treatment plan. Please arrive 10 minutes early to complete any remaining paperwork.
Will my insurance cover knee therapy?
We accept most major insurance plans, including Blue Cross Blue Shield, Medicare, Medica, UCare, Humana, UnitedHealthcare, Aetna, and PreferredOne. When you schedule, our team will verify your benefits and explain copays, coinsurance, deductibles, and visit limits. If you are uninsured or prefer self-pay, we offer transparent cash rates and flexible payment options.
What should I wear to my appointment?
Wear comfortable athletic attire such as shorts or athletic pants and a fitted top that allows full range of motion. Athletic shoes with proper support are recommended, particularly if your evaluation involves gait or balance testing. Avoid jewelry or accessories that may interfere with palpation or movement analysis.
What if I use a knee brace or crutches?
If you currently use any assistive device such as a knee brace, crutches, cane, or orthotic, please bring it to your appointment. Your therapist will assess how these devices affect your mobility and functional activities and recommend any necessary adjustments or alternative supports to optimize your rehabilitation.
How many therapy sessions will I need?
The number of sessions varies depending on the severity of your condition, your goals, and how quickly you progress. On average, patients attend physical therapy two to three times per week for four to eight weeks. We continuously reassess your progress and adjust the treatment plan and frequency accordingly. Our ultimate goal is to empower you to maintain improvements independently through a home exercise program.
Why Choose OrthoRehab Specialists for Knee Care?
- Therapist-Owned & Operated Clinics: Clinical decisions focus on patient outcomes rather than corporate targets. Our owners are licensed physical therapists who maintain high standards of care.
- Hands-On, One-on-One Treatment: You will work directly with the same therapist at every visit for personalized feedback and continuity.
- Evidence-Based Practice: We follow the latest guidelines and research from the American Physical Therapy Association and other reputable sources to deliver safe, effective interventions backed by data.
- Collaborative Referrals: Over 600 physicians, surgeons, and sports medicine specialists trust our team for post-operative care, sports injuries, chronic pain management, and prehabilitation.
- Comprehensive Services: Our clinics offer a full spectrum of knee rehabilitation options, including manual therapy, therapeutic exercise, dry needling, blood flow restriction training, functional testing, and more, tailored to each patient’s unique needs.
- Patient Education & Empowerment: We prioritize teaching you proper movement mechanics, injury prevention strategies, and home exercise techniques to ensure sustainable long-term results.
- Convenient Locations & Flexible Scheduling: Our clinics provide early morning and evening appointments to fit your busy life. Weekend slots are available on request for additional flexibility.
To learn more about our clinical philosophy and range of services, visit our Why OrthoRehab Specialists page or explore detailed treatment descriptions on our Physical Therapy Services page.
Get Started Today – Restore Your Knee Health
If you are experiencing knee pain, instability, or functional limitations, do not delay care. Early intervention often leads to faster recovery, reduced risk of long-term complications, and improved outcomes. To verify your insurance benefits or ask any questions, call our business office at 612-355-2254. When you are ready, choose your preferred booking method above to schedule your initial evaluation. We look forward to partnering with you on your path to a healthier, more active life.
